Cannabis leads us to a revolutionary molecule for addressing pain management and opioid tolerance
Marijuana, pot, weed, mary jane, cannabis; whatever you call it or however you consume it, cannabis is treasured around the world. With the widespread legalization of medical marijuana in the United States — 38 states, three territories and the District of Columbia — there’s a buzz about it among scientists. They’re trying to understand and isolate one of its magical offerings: pain relief. In one study, 30% of adults who consumed cannabis reported having used it for that reason, but they didn’t necessarily want to be high.
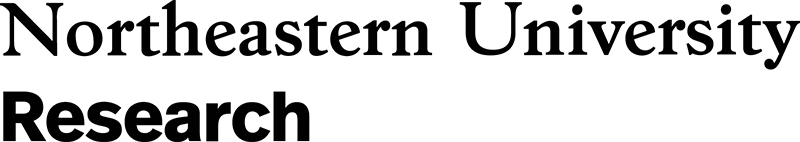
This is what propelled Alexandros Makriyannis, George D. Behrakis chair in Pharmaceutical Biotechnology at Northeastern University and director of the Center for Drug Discovery, to develop a molecule that works with the same body systems as cannabis without triggering the psychoactive effects.
“THC is nice because it’s natural and in cannabis,” he says. But he believes it’s not the only path.
Makriyannis’s first step was to understand how THC relieves pain. So, he took a deep dive into the mysterious endocannabinoid system — a network of receptors throughout the nervous system.
Here’s what he found: When someone consumes cannabis, it activates the two different endocannabinoid receptors in the brain: CB1 and CB2. The CB1 receptor produces the psychoactive outcome of cannabis and it is the most abundant receptor in the brain. CB2 affects the nervous and immune systems, making people feel more relaxed and reducing inflammation. Reducing inflammation is what reduces pain.
(The increasingly popular CBD is similar to THC, but there is no conclusive evidence that it’s effective in treating neuropathic pain).
The trick is isolating one receptor and its effects over the other.
“Initially, we had no way of distinguishing between CB1 and CB2,” says Makriyannis. “We had to produce molecules that are very selective, so we can understand what each receptor does.”
In 2011, Makriyannis and his team changed the name of the game by producing a molecule, AM1710, that works with the CB2 receptor only. The idea is that it won’t get you hooked or high. While the study worked with rats and mice, if approved by the FDA, this molecule could be manufactured into a drug that would change the lives of potentially millions of Americans who use cannabis to manage pain.
His groundbreaking study in January of 2023 built on prior research, and found something even more intriguing. Not only did the tests suggest that the AM1710 could help HIV patients suffering from peripheral neuropathy — an umbrella term for conditions that damage the nervous system — but it reversed established morphine tolerance in mice.
“[Taking AM1710] will improve the value of the opioids,” says Makriyannis. “So instead, for example, of taking five milligrams of morphine, you take only two milligrams of morphine.”
Considering the opioid use epidemic in the United States, finding a viable pain-relieving alternative would be a gamechanger. Makriyannis says that eventually, since “CB2 works against pain, it could substitute opioids.”
Before AM1710 reaches the public, it has to be refined so it’s more selective and potent. This process takes a lot of grant money and a lengthy FDA approval process. Another step will be to address the fact that in AM1710 testing, the drug worked better in male mice than in females.
Makriyannis’ interest does not stop with AM1710. He is also looking at how the CB1 receptor can be used to help people with alcoholism. He developed a molecule called AM6527 that interacts exclusively with the CB1 receptor and he is working on turning it into a drug.
“AM6527 is a very interesting molecule. It can essentially interact with the site that produces addiction and turn it off.”
He and his team at the Center of Drug Discovery recently received an $8 million grant from the National Institute on Alcohol Abuse and Alcoholism, which Makriyannis is hopeful will be enough to get this new drug tested in humans and eventually into the market.
Whether it’s improving pain management or fighting drug addiction, Makriyannis is passionate about his work, and that is made evident by how he feels about his creations.
“You see, all of these molecules are my babies. I like to see them flourish.”
Story from the Science Media Lab.
Last Updated on August 30, 2023